


The National Institutes of Health estimate that one in 200 Americans will undergo a stem cell transplant in their lifetime. Only 30 percent of patients will find a matching donor within their families, with 70 percent seeking for unrelated matching donors in the bone marrow registry.
A diagnosis of a life-threatening disease such as leukemia or lymphoma can be emotionally devastating. Often patients and their loved ones don’t know what to do first or where to turn for help. The resources presented here are intended to provide information on first steps for newly diagnosed patients whose healthcare professionals advise them that they will need a bone marrow or blood stem cell transplant.
Becoming well-informed makes it easier to take charge and advocate for yourself or a loved one.
A transplant is an infusion of healthy blood stem cells into the body to replace the ones producing the disease. Transplants can be autologous (aw-TAWL-uh-gus) meaning cells come from the patients themselves, or allogeneic (AL-oh-jen-EE-ik) meaning cells donated by another person. The type of cells used are blood stem cells, the immature cells that can grow into all types of blood cells. These stem cells may be found in three places:
The transplant collects these stem cells and infuses them into the recipient, where they migrate on their own into the bone marrow and begin the work of creating new blood cells and immune system.

Every three minutes, someone is diagnosed with a form of blood cancer like leukemia, lymphoma or myeloma. Additionally, others are diagnosed with blood disorders such as sickle cell anemia, or inherited immune disorders. For many, the only hope of a cure is a bone marrow, peripheral blood stem cell, or umbilical cord blood transplant. The diagnosis and treatment can seem overwhelming, but hope for recovery exists.
Conditions that can be treated by transplant include:

If you are diagnosed with a condition that is treatable with a transplant, you should schedule a consultation with a transplant center as soon as possible. Your physician will explain your treatment options and recommend the most appropriate type of transplant for you. If time permits, many patients seek out a second opinion about treatment.
When possible, patients are encouraged to obtain more than one opinion before choosing a hospital for treatment. Larger centers have cancer research programs in clinical, basic science, and prevention (population-based investigations) that are designated as comprehensive cancer centers by the National Cancer Institute. This ensures a strong body of interactive research leading to advances in patient treatments.
Patients have many different reasons for choosing specific transplant centers. The major considerations include:
The first step in finding a matching donor is to determine the patient’s tissue type, so that the search can be started. This means a prompt visit to a transplant center, plus starting the tissue typing search among blood relatives, in case one of them is a match. Starting an unrelated donor search in the public registries right away can also save time, and can be done by Gift of Life or by a transplant center.
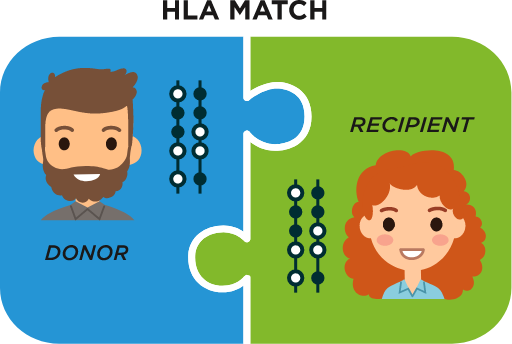
The important factor in tissue type is the Human Leukocyte Antigen (HLA), which is a complex of genes in every person’s DNA that regulates the immune system. They are also responsible for whether a transplant is accepted or rejected by the body, so a good match is crucial. Tissue typing is the laboratory process where a tissue sample collected from inside the patient’s cheek on a cotton swab (or via a blood draw) is analyzed to determine the HLA types. Ten HLA factors are determined, and once the HLAs for a patient are known, the search for a matching donor can be started.

Since HLA are a genetic factor inherited from parents, it is logical to turn first to family members and test for a match. However, because the genes we inherit are a combination from our parents, only 30 percent of those seeking a transplant match find a donor within their own family. Those who don’t find a match within the family (70 percent of patients do not find one) can search the worldwide marrow donor registries to find a match.
The worldwide registries, including Gift of Life Marrow Registry, are made up of volunteer donors who offer to become bone marrow or blood stem cell donors in the event they are determined to be an HLA match with the recipient. Searches are done through a central database called Bone Marrow Donors Worldwide, which links to registries around the world that hold the tissue type information of over 40 million volunteer donors. That sounds like a large number, yet the world population is 8 billion, so volunteer donors comprise 0.5 percent of the world population, one-half of one percent.
Perfect matches can be found in the registry, even though the donor and recipient are not siblings. When two people share an ethnic background, there is a higher chance that their HLAs will match up and the donation can take place.
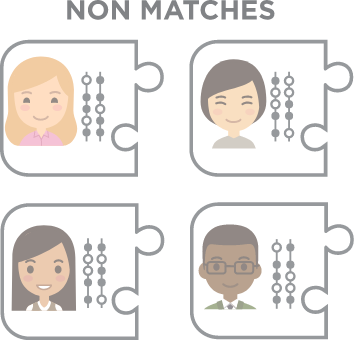

Ethnicity and ancestry play a big role in the ability to find a match – some ethnic groups are underrepresented in the registries, making it difficult for some people in need to find their match. Building the diversity of the registries is a mission of Gift of Life – adding diversity to the registry will result in more life-saving matches for those in dire need.
A haploidentical match is a half-match, for example, a biological parent is a half-match for each of their children because every child inherits half of their HLA profile from the mother and half from the father. Although half-matched transplants are rare, new advances in medicine have made the process possible for some patients under certain conditions.
Cord blood is simply collected after a baby’s birth. It is packaged and shipped to a repository where it is tested and processed, then frozen in liquid nitrogen. If a patient’s tissue type matches that of a cord blood unit, it is sent to the patient’s hospital for a transplant. Because cord blood stem cells are immature, a perfect match is not necessary.
If no match is found in the worldwide registry, that doesn’t mean no match exists, but that no one who is a match has yet registered as a donor. The family and friends of a patient can start a donor recruitment drive to try and find a match among the new donors they sign up.
Gift of Life Marrow Registry offers services to help patients’ families begin their donor search as soon as they learn a donor is needed; it is not necessary to wait until for the patient to enter the transplant center for the search to begin.
By starting the process as soon as the decision for a bone marrow or peripheral blood stem cell transplant is made, a patient and their family can be fully prepared and ready for the donor search. The faster that search can be done, the better the patient outcome.

When a patient arrives at the transplant center prepared with tissue typing information, and a family study and preliminary unrelated donor search already completed, the transplant center saves valuable time and be able to take action more quickly.
Gift of Life’s patient services include:

Being fully prepared can help ensure the timing of the transplant can happen at an appropriate time during the disease process, it allows patients to move quickly to transplant before the disease progresses or complications interfere, and allows adequate time for an unrelated umbilical cord blood search if necessary.
We believe that all patients have a donor, and we want to partner with you to find that donor as quickly as possible.

1. Share key patient information with Gift of Life as soon as possible
2. Set up Donor Drives in your community
3. Create a Gift of Life Donor Circle as a home for your search effort
We want every patient to find a matching donor and receive a lifesaving transplant. Please contact Donor Recruitment Director Chris Camacho, ccamacho@giftoflife.org, to get started.
Gift of Life provides support for patients and their families in organizing, publicizing and running donor drives, including the online tool called Donor Circles, a way to create a central hub for a recruitment drive, with tools for live tracking of results, including matches and transplants that come from among a circle’s sponsored donors.
Donor Circles offer you a way to personalize a group of donors in the Gift of Life marrow registry through your own team page. You can give the gift of test kits to your friends and family, send out e-mail broadcast invitations, blog about your journey, and more!